Funding for our most innovative research and initiatives
CUNY SPH researchers secured several major grants in 2022, funding cutting-edge initiatives that address the numerous determinants of population health.

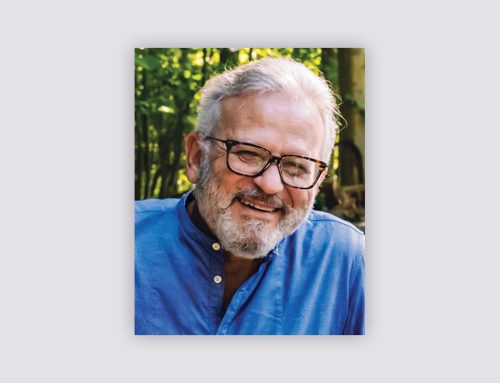
Using AI to tailor nutrition guidance for different dietary needs
Early in the year, in what is the largest single-cycle NIH grant awarded to CUNY to date, CUNY SPH and the United States Military Academy at West Point were awarded $12.4 million over five years to establish the world’s first artificial intelligence (AI) and computational modeling center for precision nutrition and health.
The center is co-led by two world-renowned AI and computational modeling experts, CUNY SPH Professor Bruce Y. Lee and West Point Professor Diana M. Thomas. Together they will develop state-of-the-art AI, machine learning, Big Data methods, and other data science approaches to better understand how different people have different dietary needs and to avoid potential biases and disparities that may result from more general, one-size-fits-all nutrition recommendations.
“This grant is part of a major NIH initiative to move our society more towards precision nutrition, better tailoring nutrition guidance and advice to different needs of people and recognizing the diversity that exists,” Lee explains. “As the AI Center for this initiative, we are at the leading edge of developing the new computer algorithms, approaches, methods, and tools that can help everyone improve their nutrition and health.”

Transmission electron micrograph of HIV-1
Methamphetamine use and HIV risk in sexual minority men
In April, CUNY SPH and the University of Miami Miller School of Medicine were awarded an initial two-year, $3,900,000 grant by the National Institute of Allergy and Infectious Diseases (NIAID) to study meth use and HIV risk in sexual minority men.
Supported by NIAID’s LITE-2 initiative, CUNY SPH Professor Christian Grov, University of Miami Professor Adam Carrico, and colleagues are examining the “where,” “how,” and “why” of meth use and HIV among men who have sex with men. For this landmark study, they will enroll 5,000 sexual minority men across the United States into a cohort study. Assuming the team can meet a series of milestones during the first two years of the study, they will become eligible for up to three more years of funding. The study’s broader goals include testing scalable, telehealth motivational enhancement interventions to support PrEP use and meth reduction. In addition, they will determine why meth use is linked to HIV vulnerability by examining if meth-induced alterations in rectal immune function amplify biological vulnerability to HIV.
“We have known for decades that meth use contributes to behavioral disinhibition, which puts people at greater risk for HIV, but now we will also answer questions related to whether meth use increases biological vulnerability,” says Grov, an investigator at the Institute for Implementation Science in Population Health (ISPH) at CUNY SPH. “This could point us toward the development of novel biomedical interventions targeting rectal immune function.”

Columbus Park in Chinatown, NYC
Park-based strategies to improve mental well-being
In September, the National Institutes of Health awarded a team of CUNY SPH researchers led by Professor Terry T-K Huang a five-year, $6.7 million grant to design and implement programmatic strategies to enhance the social environment of neighborhoods by leveraging newly renovated public parks in low-income New York City neighborhoods.
The researchers will conduct a hybrid effectiveness-implementation randomized stepped wedge trial in eight neighborhoods to determine the impact on community-level health-related quality of life and mental health of a community-engaged intervention that enables local stakeholders to design and implement programmatic strategies in the newly renovated parks.
The team will employ human-centered design (HCD), a process methodology for problem-solving and innovation, in an asset-based approach to collaborating with local partners. Specifically, each community will design one primarily physical activity strategy that promotes reach and inclusive participation among adults and one primarily social strategy—such as music, outdoor market, park beautification groups—that enhances social interaction and relationships.
“Parks are critical for neighborhood engagement and vibrancy, which in turn contribute to community well-being,” says Dr. Huang. “This study is significant both conceptually and methodologically. It pushes health disparities research from being community-participatory to community-centered, where the solutions are community-driven and based on authentic community needs, values and culture.”

Applying a novel opioid intervention platform
In October, The National Institutes of Health awarded a two-year, $1,147,508 grant to CUNY SPH Associate Professor Nasim Sabounchi and Yale School of Medicine Assistant Professor Rebekah Heckmann to test a new evidence-based intervention that links people who have overdosed with access to medication for opioid use disorder, harm reduction services and recovery supports.
Sabounchi, Heckmann, and colleagues will implement a comprehensive telehealth platform that can be deployed at the site of an overdose or in the emergency department with minimal time or effort by existing staff. The platform will provide real-time access to providers who prescribe medication for opioid use disorder and other harm reduction services for high-risk individuals and may remove many of the barriers to follow up that these individuals face.
The researchers will collect high-quality data about the processes and outcomes associated with deployment of this platform in Connecticut that can be integrated with their existing system dynamics model to determine how or whether interventions should be implemented more broadly in the future.
“There is a great need to expedite and facilitate access to medication for opioid use disorder and respond effectively to witnessed overdoses,” says Sabounchi. “Our long-term goal is to implement these novel system dynamics modeling and telehealth strategies in Connecticut, with subsequent dissemination nationally, ultimately improving access to medication and reducing overdose events and fatalities.”