The finger-prick, painful but necessary, draws the blood sample that will reveal whether the wailing child has been exposed to lead, a known neurotoxin that can cause permanent intellectual disability in children subjected to it prenatally or in early childhood.
If so, then a venous blood draw will follow to confirm the initial results, as well as further testing, and treatment. The procedures are invasive, costly, time consuming and, according to preliminary research from the Department of Environmental, Occupational, and Geospatial Health Sciences at CUNY SPH, potentially avoidable.
By analyzing meconium from a robust sample of newborns in hospitals across New York City, Associate Professor Brian Pavilonis, Professor Suzanne McDermott, and colleagues found detectable levels of lead, plus nine other metals which, in high concentrations, are associated with a host of biological and neurodevelopmental problems. In addition to using meconium—instead of blood—as a biomarker for measuring women’s prenatal exposures to potentially toxic metals, the study identified environmental contamination in a few geographic areas of the city. This will help establish a baseline of metal concentrations among representative populations in the city which, in turn, may help healthcare providers and mothers of newborns catch elevated environmental exposures early enough to minimize and even avoid their effects.
“The study adds to the literature a cheap, easy, and effective way to measure metal concentrations in newborns, and to identify early exposures that can allow you to do an intervention,” Pavilonis says. “Right now, we do not know what constitutes ‘elevated’ levels of metals in meconium, and that is one of the goals of the project: to determine average concentrations of metals in NYC so in the future we can detect outliers.”

Meconium, a thick, dark green or black substance, is the first stool that newborns pass. Its production begins early in the second trimester of pregnancy, and so it reflects several months of accumulated maternal-fetal environmental exposure, explains McDermott, who has extensively studied and written about the relationship between toxic environmental exposures and neurodevelopmental disabilities, including intellectual disability and autism. “Meconium captures the past three to six months of maternal-fetal exposure, unlike cord blood, which captures the past week’s,” she says.
The cross-sectional pilot study, which the researchers conducted in cooperation with physicians from the New York City Health and Hospital system (NYCHHC), analyzed meconium samples from 124 newborns within the first 24 hours of delivery at five NYCHHC hospitals: Elmhurst and Queens hospitals in Queens; Jacobi Hospital in the Bronx; Kings County Hospital in Brooklyn; and Metropolitan Hospital in Manhattan. The study team provided special diapers for meconium collection and helped to recruit the mothers and gain their verbal consent to participate in the study. The mothers spoke a range of languages that reflected the ethnic and language diversity in the hospitals’ catchment areas. All qualified to participate, regardless of their primary language, as long as their infant had not passed its first feces. If English was not a woman’s first language, then a closed-circuit hospital phone translator explained the study and obtained her consent.
Most of the quantifiable meconium samples came from full-term infants, and only a small number came from those born pre-term, before 37 weeks. All study subjects remained anonymous. The only personal data that researchers gathered was the zip code where each mother lived during her pregnancy, and each infant’s gestational age and birthweight.
Of the 124 samples, 116 had enough meconium to conduct analytical analyses. In the meconium, researchers found detectable levels of nine metals: cadmium, chromium, copper, iron, manganese, molybdenum, nickel, lead, and zinc. Possible sources for elevated levels of these metals, in addition to diet, include emissions from power plants and waste incineration, exhaust from trucks and cars, deteriorating housing, and nearby brownfields. All but two samples contained measurable amounts of lead, while approximately half contained measurable levels of cadmium.

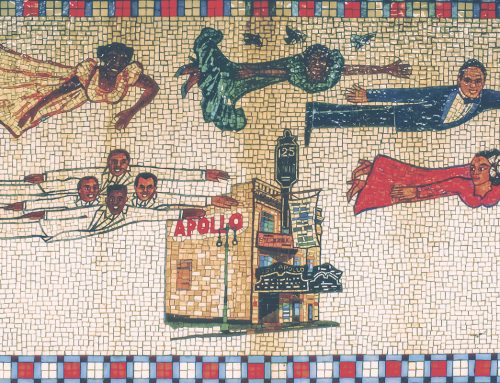
Published by the Merchants’ Association of New York in 1922—this map shows the various types of industry that once existed across the city. This deep history of manufacturing is one of the reasons why elevated metal levels can be detected in soil samples across the boroughs. CREDIT: New York Public Library
The study also identified “hot spots” for various metal combinations. For example, in the meconium of southeast Brooklyn newborns, researchers detected copper, zinc and iron; they found cadmium, chromium, and nickel in the meconium of babies born in eastern Queens; and they found aluminum and molybdenum in the meconium of babies born in south Queens. In the south Bronx, they found increased concentrations of lead.
“Numerous studies have measured metal concentrations in meconium samples, but this study was unique due to the large number of metals it quantified, with different sources and biological need, among a convenience sample from a large urban population,” Pavilonis, McDermott, and their team wrote in a paper that will appear in an upcoming issue of the Environmental Research Journal. “The fact that 39.7 percent of the samples had concentrations of the ten metals above the laboratory limit of detection suggests that metal exposures are abundant in NYC,” they wrote.
New York City, once a major industrial and manufacturing center, has a long history of metal contamination, Pavilonis explains. Over several decades, industrial byproducts, and other contaminants have accumulated to create the currently elevated levels of copper, zinc, and lead in soil citywide.
Most people are exposed to some level of the metals that the study found in meconium, says Pavilonis, an environmental health scientist and certified industrial hygienist. In fact, some metals, like copper, iron, manganese, molybdenum, and zinc are nutritionally necessary trace elements for pregnant women and their fetus. “During different phases of fetal growth, different nutrients are needed for development, so we do not want to completely eliminate exposure,” he says. “Copper, manganese, zinc, iron, and chromium are all nutritionally necessary for growth and development.”

A vacant lot in NYC. Deteriorating buildings and vacant lots/brownfields are possible sources for elevated metal levels in meconium. CREDIT: Nils Agrell

The Brooklyn-Queens Expressway in NYC. Vehicle exhaust is another possible source of elevated metal levels. CREDIT: Paul McGeiver
At high concentrations, however, these metals are associated with a host of problems, including decreased birthweight, gestational diabetes, preeclampsia, preterm birth, intellectual disability, and autism.
“Neurodevelopmental disabilities are all multi-factorial, but we believe these metals are in the pathway that causes genetic changes that are associated with intellectual disability and autism,” McDermott says.
For example, the study found an association between lead concentrations and decreased birthweight. Lead, in particular, competes with calcium in the body. When women are exposed to lead, it enters their bones in the same way that calcium would, McDermott explains. During pregnancy, the normal process of drawing calcium from maternal bones to support fetal development also draws lead from these exposed women. Thus, in utero exposure to lead can lead to cascading physical and mental outcomes, including neurodevelopmental disabilities that are associated with reduction in the infant’s intelligence quotient (IQ). In addition to lead, aluminum and cadmium are toxic to the human body, and can cause permanent brain damage, she adds.
The problem is that there is no baseline data for what constitutes ‘elevated’ or ‘dangerous’ levels of individual metals. “It’s important to figure out when a metal that your body needs becomes too much of a good thing,” McDermott says. “We don’t know what those levels are. We’re trying to figure it out.”
Moreover, there is no data on the biological effects of metal combinations.
“Metal mixtures are always problematic,” Pavilonis says. “With a mixture comes the potential synergistic or additive health effects that can occur at lower concentrations than those resulting from individual metals,” he says.

The study found some of the highest metal concentrations in some of New York City’s most socially and economically distressed geographic areas, which typically have high rates of racial and ethnic disparities in health and health care. For instance, Pavilonis notes, “Increased lead concentrations were detected in the South Bronx area, which also has a long history of poor health outcomes and racial, ethnic, and economic disparities.” The mothers in the study largely had low incomes and either government-subsidized or no health insurance, McDermott says. “The babies were most likely to have had exposures because of their parents’ occupations, the place where they lived, or natural disadvantage,” she says.
Linking socioeconomically disadvantaged neighborhoods with toxic environmental exposure is a major benefit of the study, as it may eventually help healthcare providers offer patients ways to lower their risk of exposure by asking the health department to inspect their homes for lead, keeping their floors free of dust, which often contains breathable metal particulate, and using a HEPA filter at home to reduce airborne dust.
“Ideally a child should never be exposed to lead, but you want to catch the exposure as early as possible to try to remediate situation, so you might send mom home with tips on how to lower lead exposure,” Pavilonis says. “If elevated mercury is found, then an individual should consider changing their diet and consuming less fish.”
One of the study’s greatest values is its identification of meconium as a reliable biomarker for measuring fetal exposure to toxic contaminants, says neonatologist Nadine M. Lahage one of the study’s NYCHHC co-researchers.
“This study has shown that metals are detectable in the meconium of NYC newborns, indicating exposure during the pregnancy via transplacental passage,” Dr. Lahage says. “Mothers can be exposed through various sources such as food, water or maybe skin products. Refining these results and correlating with neonatal health outcomes may help us find ways to prevent adverse neonatal outcomes related to metal exposure in NYC.”
Analyzing meconium is also more cost efficient than analyzing blood. Whereas a traditional approach to researching metal exposure would entail, among other things, paying a trained phlebotomist to draw blood and subjecting an infant or child to a blood test, meconium analysis is neither costly nor invasive.
“It’s easy for a trained individual to collect, which improves subject participation and decreases collection costs,” Pavilonis says.
He and his team have applied for funding from the Environmental Protection Agency to expand their current study into one that looks specifically for associations between metal mixtures and potential changes in the mother and child’s genetic code. They are also working on a grant to study whether fetal exposure to disinfectants increased during the height of the pandemic, when so many people were isolating at home. Pavilonis is also collaborating with Associate Professor Andrew Maroko on a study that examines how blood lead levels from specific zip codes correspond to lead in the soil.
For the present, however, they hope their establishment of meconium as a non-invasive, low-cost, and more comprehensive biomarker than blood for measuring maternal-fetal exposures to metals will give women the information they need to reduce theirs. Says Pavilonis, “We need to develop tools that are cheap and can be done quickly to assess fetal exposure to metals, and this is a good way to do it.”