Pictured above, doctoral student Matthew Romo
In 2018, nations and health organizations around the world suspended use of dolutegravir, the top HIV antiretroviral treatment for women of reproductive age.
The dramatic move came after the World Health Organization (WHO) cautioned about the drug after reporting from Botswana on nervous system defects in newborns of women who had become pregnant while on the therapy.
Yet, even after later data provided reassurance about the safety of the drug, only half as many women as men were accessing it in 2020, meaning millions were still going without it, and still may be.
The fallout from that 2018 statement is the subject of new research published in January in Annals of Internal Medicine by Matthew Romo, a CUNY SPH doctoral student in epidemiology and a pharmacist interested in HIV.
“It points to the need to strike the right balance between simultaneously protecting and promoting public health,” says Romo. He notes that in many countries, women were effectively denied access to a best-in-class drug—even if they were using contraception and didn’t plan to have children—based on an extremely low-risk and still uncertain event. “The lesson here is that the affected population, women living with HIV, should have been part of the decision to access the drug.”
Romo’s research is part of a larger body of work around the study of HIV treatment and care at CUNY SPH. Denis Nash, Romo’s dissertation adviser, is principal investigator for the Central Africa region of the International epidemiology Databases to Evaluate AIDS (IeDEA), a consortium of countries in the Americas, Africa, and, Asia-Pacific that collect observational data on 2.2 million people living with, or at risk for HIV. Through Nash, Romo was able to access this large dataset and collaborate with international investigators to research the extent of the impact the decision to suspend dolutegravir had on women.
“Matt’s landmark research studies have immediate implications for policy and practice vis-à-vis the persisting disparities in the ongoing global dolutegravir rollout,” says Nash, who is also executive director of the CUNY Institute for Implementation Science in Population Health (ISPH) and distinguished professor of epidemiology at CUNY SPH. “Matt brought his unique lens from his training as a pharmacist and as an epidemiologist. It allowed him to take a very broad research priority and focus it in some very important and relevant ways,” Nash adds.

Denis Nash
According to Annette H. Sohn, Vice President, amfAR, The Foundation for AIDS Research and chair of the IeDEA Executive Committee, “Matt’s research has provided us with valuable benchmarks for early real-world experiences in rolling out dolutegravir treatment using IeDEA data. He successfully navigated IeDEA’s complex consortium, and ably managed our multi-regional data to produce high-impact science.”
Over the last 25 years, improvements in antiretroviral therapy have made it possible for people with HIV to have long, healthy lives and drastically reduced the risk of transmitting the virus. Even in this landscape, dolutegravir, “represents a new era for HIV treatment,” says Romo. Patients on the drug, which is taken once a day as a tablet combined with other antiretroviral medications, are able to more strongly suppress HIV and are less likely to develop resistance, compared to the previous preferred first-line antiretroviral, efavirenz. Individuals also experience fewer side effects, making them less likely to discontinue use. Importantly, because of improved viral suppression, the risk of transmitting HIV is also reduced.
For these reasons, the WHO first recommended dolutegravir as part of first-line antiretroviral therapy in 2016. But in May 2018, a study out of Botswana changed access to the drug for millions of women. In that country, four newborns of 426, or about 0.9 percent, were born to women who became pregnant while on the therapy and had defects in the brain, spine, or spinal cord, known as neural tube defects. In comparison, the risk of neural tube defects was 0.1 percent among infants born to women taking other antiretroviral regimens at the time of conception.
This kind of event, known as a “post-marketing safety signal,” refers to when reporting has shown an adverse effect in people who take a medicine after it becomes available to the public, but more investigation is needed to determine if the medicine is the cause.
In response, the WHO cautioned against use of dolutegravir for women of reproductive age and called for further investigation. Following the agency’s action, countries and organizations largely restricted access to the treatment for women in that group.

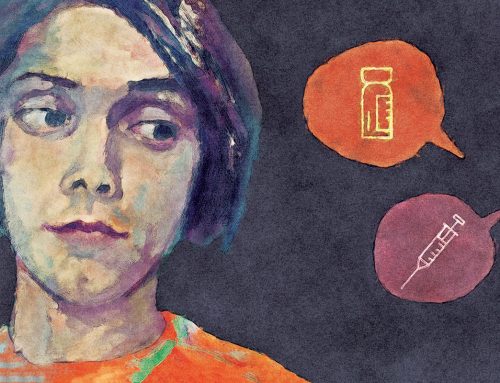
In 2018, a study out of Botswana reported that almost 1% of children born to mothers taking the antiretroviral drug dolutegravir resulted in neural tube defects. Subsequent, larger studies did not find this risk.
More data from Botswana later showed the risk of neural tube defects was even lower than in the initial report—0.3 percent with dolutegravir vs. 0.1 percent with other antiretrovirals. Additionally, pregnancy surveillance studies from other countries did not identify an increased risk of neural tube defects. According to researchers’ models, dolutegravir’s benefits in reducing both deaths among women and HIV transmission outweighed the low potential risk of neural tube defects.
This led the WHO to reverse its decision in July 2019 and recommend the drug again for all people living with HIV, but the initial action is still reverberating around the world. (The most recent data from Botswana have shown that dolutegravir is no longer significantly associated with an increased risk of neural tube defects—effectively putting the safety issue to rest.)
Yet, for every 100 men ages 16 to 49 that initiated dolutegravir, only 51 women of the same age did so through 2020, as Romo discovered from analyzing data on 134,672 patients at 87 facilities in Brazil, Cambodia, Kenya, Rwanda, Uganda, Democratic Republic of the Congo, Haiti, Lesotho, Mozambique, Tanzania, and Zimbabwe, through the IeDEA registry.
The safety signal had an especially significant impact on sub-Saharan Africa, where women of reproductive age are the population most affected by HIV. According to the Joint United Nations Programme on HIV/AIDS (UNAIDS), young women in the region ages 15 to 24 are twice as likely to be living with HIV than men.

A colorized scanning electromicrograph of an HIV-infected H9 T cell. CREDIT: NIAID
“Countries were pretty quick to restrict access,” says Romo. “To reverse things, it’s much harder. It takes a long time. Policies need to change and countries must figure out how to implement these guideline changes through supply chains. Questions and concerns among clinicians and people living with HIV must also be addressed.”
The study spotlights the consequences of responding to a safety signal too restrictively and leaving those most affected out of the decision-making process.
“Even if there is potentially a slightly elevated risk of birth defects, does this outweigh the known benefits of viral suppression and reduced mortality and HIV transmission?” Romo asks. “The scales were really tipped in favor of the known benefits versus a very small, uncertain risk when considering if access to the drug should be restricted.”
The episode also points to the need for pregnant women to be better represented in clinical trials, where risks could be identified earlier. Leaving pregnant women out of trials is often justified because of unknown risk to the mother or the fetus. But nonclinical reproductive and developmental toxicity studies done before the human subject phase of the trial can help identify whether a drug is potentially unsafe for pregnant women or women who become pregnant, according to Romo.
“Romo and colleagues provide a poignant example of how far we remain from prioritizing women’s decision-making autonomy and health and from having timely, high-quality data for drugs used during pregnancy and breastfeeding,” an editorial published with Romo’s study in Annals wrote.
As Romo says, “Women will eventually take the drug in real life, so we owe it to them to provide relevant safety and efficacy data before it comes to market. We need to protect people through research not from research.”
The question of how to weigh uncertain safety issues with known clinical benefits has also become more pressing with the sensitivity of communication around COVID-19 vaccines.
“It takes a long-time to address concerns and restore trust, even after new, reassuring data comes out,” Romo says.
During his undergraduate studies in 2005, Romo got a job as a research assistant on a clinical trial of new HIV treatments at Cedars Sinai Medical Center in Los Angeles.
“It was a time during the HIV epidemic when treatment was just beginning to be expanded globally,” said Romo. “It was a phenomenon that was saving lives in high-income settings, like the United States, Canada, and Europe, but millions of people globally were not yet on treatment.”
He went on to earn a Doctor of Pharmacy degree at Massachusetts College of Pharmacy and Health Sciences in Boston, and gained experience in HIV clinical treatment through a clinical clerkship at Beth Israel Deaconess Medical Center in Boston and a volunteer opportunity with Fundación Huésped in Buenos Aires, Argentina.
He began a master’s in public health in 2012 at what was then the Urban School of Public Health at Hunter College, (before CUNY SPH became an independent school).

“Matt demonstrated a proclivity for academia even before joining the doctoral program in epidemiology,” says Associate Professor Elizabeth Kelvin, Romo’s MPH mentor. “His coursework while an MPH student resulted in at least four publications in peer reviewed journals that I am aware of; and he has sought out academic opportunities in institutions around the world. I know that he will continue to be an excellent academic and colleague.”
Romo went on to work as a consultant for the New York City Department of Health and Mental Hygiene’s Bureau of Epidemiology Services, and as a visiting researcher at the University of Cuenca School of Medicine in Ecuador. During his doctoral study, which he began in 2016, he has taught epidemiology classes and mentored students at CUNY SPH and The University of Hong Kong, where he lived with his husband for three years before moving back to the U.S. He earned his PhD this spring.
“Matt has great ability to synthesize and present data in a concise way,” says Pui Ying (Polly) Chan, City Research Scientist at New York City Department of Health and Mental Hygiene, who is a friend. “He is also gifted in scientific writing, which is attested by his long list of publications to date.”
Romo defended his doctoral dissertation successfully this February. He’ll stay on with ISPH, work on submitting a National Institutes of Health K01 training grant, and continue to study the effects of HIV treatment on populations. He hopes eventually to be faculty at a university because of his love of research and mentoring students.
“At CUNY SPH, I’ve had the best mentorship I could ask for,” says Romo. “My hope as a researcher is to pass that on to other researchers in the future.”

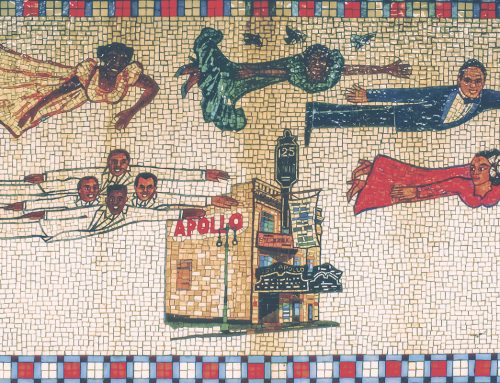
Maggie Medison, 18, from Malawi, dropped out of school in 2015 because she became pregnant. She represents the group most affected by the safety signal. She now works in her community to raise awareness about the importance of remaining in school and protecting against HIV. CREDIT: Josh Estey/USAID